Abstract
Background: Multiple myeloma (MM) treatment facility volume, an indirect measure of treating physician experience with the disease, has been shown to affect mortality (Go et al, JCO 2016). Since MM is commonly treated with autologous stem cell transplantation (AUTO-SCT), we set out to explore if annual facility volume of AUTO-SCT had an impact on survival outcomes. We additionally explored if hospital volume or public/private hospital type had an effect on hospitalization cost among this patient population.
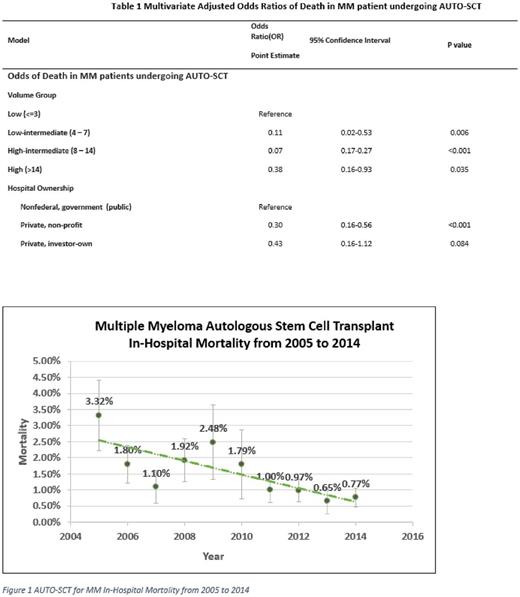
Methods: The Nationwide Inpatient Sample (NIS) is a validated database of discharges from a representative sampling of U.S. hospitals excluding rehab facilities and federal hospitals. Using the NIS, we identified adult patients hospitalized with ICD-9 codes for AUTO-SCT and MM from 2005 to 2014. Hospitals were divided into four similar sized groups based on the number of patients who received AUTO-SCT for multiple myeloma per year: low-volume (L) <=3; low-intermediate volume LV = 4-7; high-intermediate volume (HV) = 8 - 14; and high volume (H) >14). Public (non-federal government) hospitals and Private, non-profit and for-profit hospitals were assessed separately. We used trend analysis to evaluate hospitalization mortality and hospitalization cost over the study period. We used logistic regression to determine associations between mortality and hospital volume or public/private hospital type among patients with MM, adjusting for year of admission, demographics (gender, race, age), socioeconomic variables (income, insurance), geography (facility location), institution type (facility ownership, teaching hospital status), and comorbidity (Charlson comorbid score). We used multivariate regression to determine volume to cost and public/private hospital to cost associations adjusted for the same variables and also for inflation rate and length of stay.
Results: We identified 8183 patients in the NIS database, which was equal to an estimated 39,971 nationwide admissions for AUTO-SCT for MM from 2005 to 2014. The median age for all admitted patients was 58.9 years and 57.1% were men. The median hospital volume was 12.94 patients per year. In-hospital mortality decreased to < 1% from >3% over the study period (Figure 1, p=0.002). The distribution of patients according to hospital volume was L: 4.45%, LV: 9.31%, HV: 17.34% and H: 68.3%. The unadjusted mortality was: L: 2.52%, LV: 0.37%, HV: 0.51%, and H: 1.79%. No crude length of stay difference was observed between low-volume hospitals and higher-volume hospitals. Patients who received autologous stem cell transplantation in higher-volume hospitals had lower in-hospital mortality (odds ratio: 0.27 [95% CI, 0.11-0.26]). We further looked into each individual group and found that patients treated at higher-volume hospitals all had a lower risk of death (Table 1). When compared to public hospitals, mortality risk for MM patients who received AUTO-SCT was lower at private non-profit hospitals (OR: 0.30 [95% CI, 0.16 to 0.56], p<0.001) and not significantly different in private for-profit hospitals (OR: 0.43 [95% CI, 0.16 to 1.12], p=0.08). The overall hospitalization cost of AUTO-SCT corrected for inflation decreased during the study period (p=0.03). No cost differences were found between low-volume hospitals and higher-volume hospitals. Costs at both private non-profit and for-profit hospitals were lower compared to public hospitals (p<0.001 and p=0.003, respectively).
Conclusion: Mortality and inflation-adjusted costs for AUTO-SCT for MM have gone down over the past decade. Patients who receive AUTO-SCT for MM at low-volume or public hospitals face a higher risk of mortality compared to those at higher-volume hospitals or private non-profit hospitals. Hospitalization costs at private hospitals are lower than public hospitals. Analysis of the NIS database reveals significant nationwide differences in costs and mortality risk for MM patients undergoing AUTO-SCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal